What Mpox really is?
Mpox, formerly known as monkeypox, is a viral zoonotic disease caused by the mpox virus, which belongs to the Orthopoxvirus genus, the same genus as the smallpox virus.
a
The disease is not new and has been known since its first discovery in 1958, the virus was first identified in 1958 in research monkeys in Denmark, which is how it got its initial name.
a
The first identification of the mpox virus is in research monkeys in Denmark and the first recorded human case is in the Democratic Republic of the Congo (DRC), it can seem puzzling, but here’s how it makes sense;
a
- Importation of Monkeys: During the late 1950s, it was common for research institutions in Europe and the United States to import primates from Africa for scientific research. The specific origins of the monkeys used in the 1958 research in Denmark are not always explicitly documented, but the suspicion is based on the general practice of importing African primates for research.
- Endemic Nature of the Virus: Mpox is known to be endemic in Africa, where it naturally infects animals such as rodents and some primates. Therefore, the presence of the virus in monkeys used for research would fit with the known distribution of the virus.
Is it similar to smallpox ?
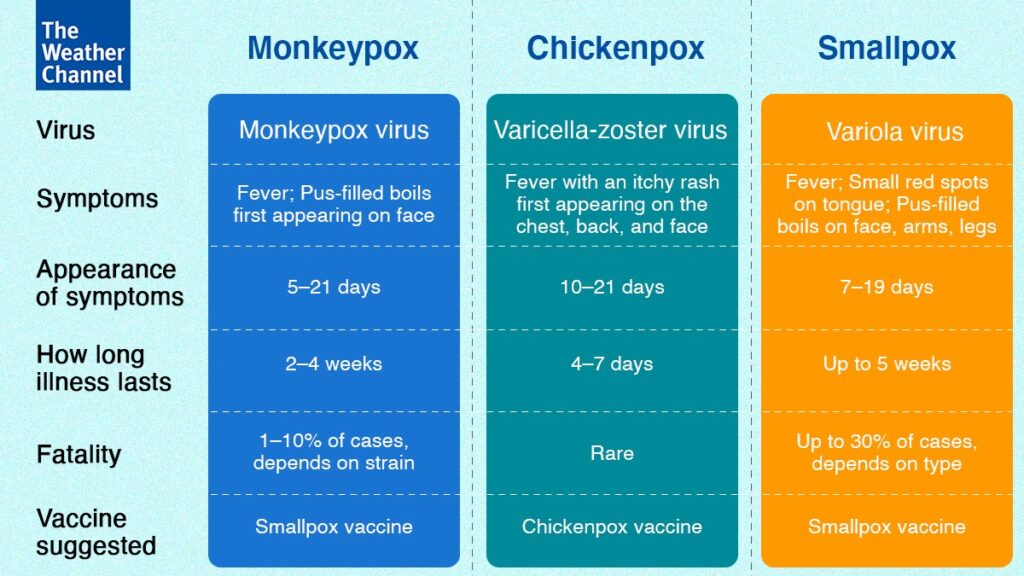
Mpox (formerly known as monkeypox) and smallpox are not the same, but they are related. Here’s a breakdown of their similarities and differences:
a
Similarities:
- Virus Family: Both mpox and smallpox are caused by viruses from the Orthopoxvirus genus. Smallpox is caused by the variola virus, while mpox is caused by the mpox virus (previously called the monkeypox virus).
- Symptoms: The symptoms of both diseases can be similar, including fever, body aches, and a characteristic rash that turns into pustules. However, the severity and progression of these symptoms can differ.
- Transmission: Both viruses can spread through close contact with infected individuals, including through respiratory droplets, bodily fluids, and contaminated objects.
Differences:

1.Severity: Smallpox was much more severe and had a higher fatality rate compared to mpox. Smallpox had a fatality rate of around 30%, whereas mpox typically has a lower fatality rate, ranging from 1% to 10% depending on the clade (strain) of the virus.
2. Eradication: Smallpox was declared eradicated in 1980 following a successful global vaccination campaign. Mpox, on the other hand, still occurs, particularly in Central and West Africa, though it has also caused outbreaks in other parts of the world.
a
3. Host Species: Smallpox only infects humans, while mpox can also infect various animals, particularly rodents and non-human primates. This animal reservoir makes it more difficult to control and eradicate mpox.
a
4. Vaccine: The vaccine developed for smallpox (vaccinia vaccine) is also effective against mpox, which is why vaccination efforts can help control mpox outbreaks.
a
a
What is 2022 Mpox outbreak?
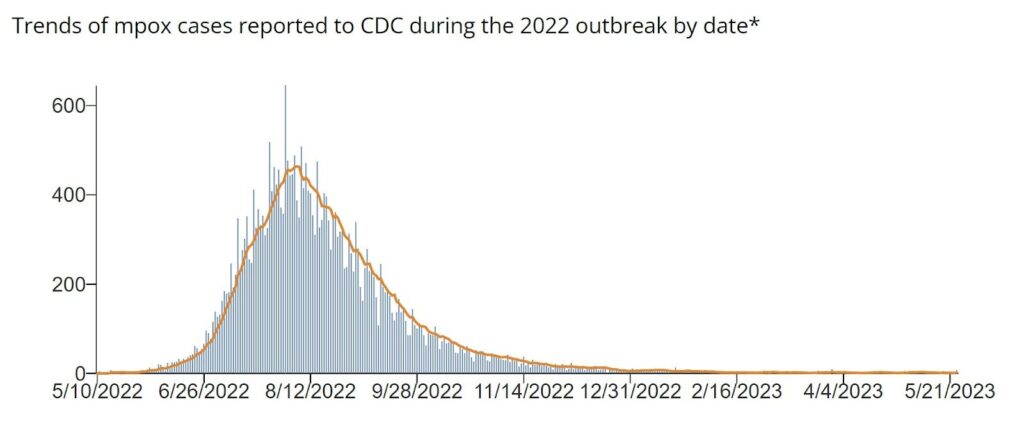
In May 2022, the World Health Organization made an emergency announcement of the existence of a multi-country outbreak of mpox, a viral disease then commonly known as “monkeypox”.
a
How did we overcome the 2022 outbreak?
1. Vaccination Campaigns:
- Increased Availability: Efforts were made to increase the availability of mpox vaccines, including the Modified Vaccinia Ankara (MVA) vaccine, which provides protection against mpox. Vaccination campaigns targeted high-risk populations, including those in outbreak areas and individuals with close contact to infected persons.
- Global Distribution: Vaccines were distributed to countries experiencing outbreaks, and public health organizations coordinated to ensure equitable access, especially in regions with limited resources.
2. Public Health Measures:
- Isolation and Quarantine: Infected individuals were isolated to prevent further spread. Public health authorities also implemented quarantine measures for those who had been in close contact with infected persons.
- Contact Tracing: Comprehensive contact tracing was conducted to identify and monitor individuals who had been exposed to the virus, helping to prevent secondary cases.
- Public Awareness: Public health campaigns were launched to educate people about mpox, its symptoms, and preventive measures. This helped to increase awareness and encourage early detection and treatment.
3. International Cooperation:
- Global Health Response: The World Health Organization (WHO) and other international health bodies coordinated the global response, providing guidance, resources, and support to affected countries.
- Sharing Information: Data and information about the outbreak were shared internationally to enhance understanding of the virus and improve response strategies.
4. Surveillance and Monitoring:
- Enhanced Surveillance: Surveillance systems were strengthened to monitor the spread of mpox and detect new cases quickly. This allowed for timely interventions and updates to public health guidelines.
- Ongoing Monitoring: Even as the initial surge of cases was controlled, ongoing monitoring continued to ensure that the virus did not resurge or cause new outbreaks.
5. Containment and Resolution:
- Decline in Cases: With effective vaccination, public health measures, and international cooperation, the number of new cases declined significantly. The outbreak was declared under control in many areas, with cases becoming more sporadic.
- Focus on Preparedness: Efforts shifted towards ensuring that the necessary infrastructure and preparedness measures were in place to manage any future cases and prevent potential resurgences.
Current Status:
- Continued Vigilance: While the immediate crisis of the 2022 outbreak has been addressed, continued vigilance and preparedness are necessary. Health authorities remain attentive to potential new cases and maintain surveillance to manage any future outbreaks effectively.
If it is discovered in 1958, overcame in 2022 and the fatality rate is low why is it so important now in 2024 ?
1. Recent Global Outbreaks:
- The significant increase in cases and global spread of mpox starting in 2022 has drawn attention. This marked the first time the virus spread widely outside its traditional endemic regions in Africa, leading to a global health response.
2. Increased Transmission:
- Mpox has demonstrated the ability to spread more effectively in new populations, including through close human-to-human contact, which was less evident before. This has raised concerns about the potential for sustained outbreaks and transmission in previously unaffected areas.
3. Vaccination Coverage:
- Although smallpox vaccination provides some protection, many people, especially those born after the eradication of smallpox, are not vaccinated. This gap in immunity increases the risk of mpox spreading among unvaccinated populations.
4. Public Health Infrastructure:
- The recent outbreaks have highlighted gaps in public health infrastructure, including surveillance, response capabilities, and vaccine distribution. Addressing these gaps is crucial for managing current and future infectious diseases.
5. Global Health Security:
- The mpox outbreaks serve as a reminder of the importance of global health security and preparedness for emerging infectious diseases. The response to mpox is part of broader efforts to strengthen global health systems and improve response strategies.
6. Potential for Complications:
- While the fatality rate is lower compared to some other viruses, mpox can still cause severe health complications, particularly in vulnerable populations. These complications require ongoing attention and healthcare resources.
7. Public Awareness:
- Raising public awareness about mpox, its symptoms, and prevention methods is crucial for controlling its spread. The recent outbreaks have increased the need for education and communication to prevent further cases.
8. Research and Development:
- Ongoing research into mpox helps improve understanding of the virus, develop better treatments, and refine vaccines. The recent global focus has accelerated efforts in these areas.
In summary, while mpox has a low fatality rate, its importance now stems from recent global outbreaks, the potential for increased transmission, gaps in vaccination coverage, and the need for continued public health vigilance and preparedness.
a
What are the signs and symptoms of mpox?
After exposure, it may be several days to a few weeks before you develop symptoms. Signs of mpox include:
- Fever.
- Rash.
- Swollen lymph nodes.
- Chills.
- Headache.
- Muscle aches.
- Fatigue.
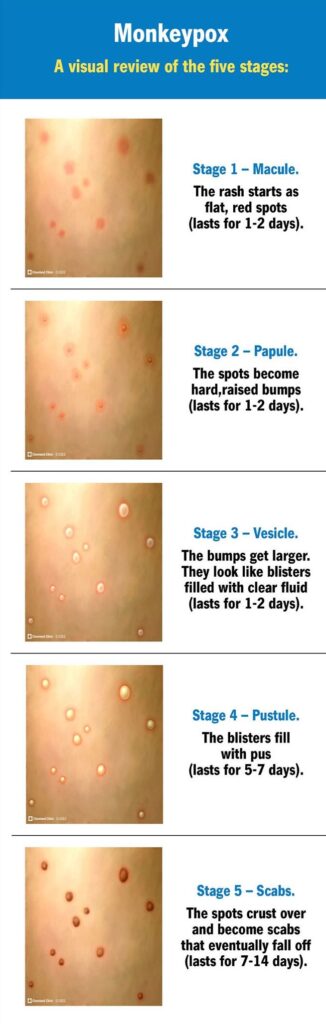
The rash starts as flat, red bumps, which can be painful. Those bumps turn into blisters, which fill with pus.
a
Eventually, the blisters crust over and fall off. The whole process can last two to four weeks. You can get sores on your mouth, face, hands, feet, penis, vagina or anus.
World trends
Globally, the most affected region in June was Africa, with 567 cases of infection, followed by the Americas (175 cases), Europe, excluding the Eastern Mediterranean region (100 cases), Western Pacific (81 cases) and Southeast Asia (11 cases).
a
From 1 January 2022 to 30 June 2024, a total of 99,176 laboratory-confirmed cases of mpox, including 208 deaths, have been reported to the UN health agency from 116 countries in all WHO regions. Apart from Africa, “the outbreak continues at a low level of transmission” globally, WHO said.
a
Data for June indicated that 16 out of 26 reporting countries showed an increase in cases compared to May. DR Congo reported the highest increase in Africa, with 543 cases in June compared to 459 a month earlier (up 62 per cent), while Spain saw the highest increase in Europe (54 cases, up from 38 in May), Colombia reported the highest increase in the Americas, with 11 cases in June and none in May, and Australia had the highest increase in the Western Pacific (from 33 cases in May to 64 in June). No country reported an increase in Southeast Asia.
a
aa